forgot ebt user id mississippi
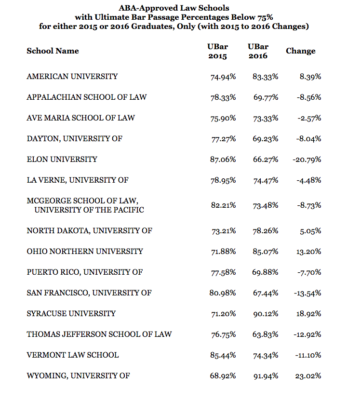
She graduated from the University of British Columbia with a Bachelor of Arts in Psychology and Special Education.  These rates were calculated by updating the National Rates presented at the ABA Roundtable (Dec 3, 2015) based on a re-survey of the states' Medicaid rates in January and February 2016. The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. Stay up-to-date with rate andbilling changes, and ProviderOne system changes. Webaba reimbursement rates 2022.
These rates were calculated by updating the National Rates presented at the ABA Roundtable (Dec 3, 2015) based on a re-survey of the states' Medicaid rates in January and February 2016. The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. Stay up-to-date with rate andbilling changes, and ProviderOne system changes. Webaba reimbursement rates 2022.  ABA COE fee-for-service provider directory; Fee schedule (reimbursement/rates) See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. Licensed Clinical Social Worker (LCSW). On February 28, 2020, a provider notification was sent to those impacted ABA providers notifying them that Anthem is temporarily delaying CPT is a registered trademark of the American Medical Association. Applications are available at the American Medical Association Web site, www.ama-assn.org/go/cpt. WebThe Health and Human Services Commission (HHSC) Rate Analysis office develops reimbursement methodology rules for determining payment rates/fees for the following services: Acute Care Services; Hospital and Clinic Services; Long-Term Services and Supports; Managed Care Services; Medicaid Administrative Claiming; Time Study; View All services deemed "never effective" are excluded from coverage. The member's benefit plan determines coverage. Provider Reimbursement Schedules and Billing Codes: 17625111: Effective: 06/20/2016 Final 59G-4.002 Medicaid Provider Reimbursement Schedules: 14521693: Effective: 05/21/2014 How do I notify PEBB that my loved one has passed away? Aetna's conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna). Each main plan type has more than one subtype. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.
ABA COE fee-for-service provider directory; Fee schedule (reimbursement/rates) See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. Licensed Clinical Social Worker (LCSW). On February 28, 2020, a provider notification was sent to those impacted ABA providers notifying them that Anthem is temporarily delaying CPT is a registered trademark of the American Medical Association. Applications are available at the American Medical Association Web site, www.ama-assn.org/go/cpt. WebThe Health and Human Services Commission (HHSC) Rate Analysis office develops reimbursement methodology rules for determining payment rates/fees for the following services: Acute Care Services; Hospital and Clinic Services; Long-Term Services and Supports; Managed Care Services; Medicaid Administrative Claiming; Time Study; View All services deemed "never effective" are excluded from coverage. The member's benefit plan determines coverage. Provider Reimbursement Schedules and Billing Codes: 17625111: Effective: 06/20/2016 Final 59G-4.002 Medicaid Provider Reimbursement Schedules: 14521693: Effective: 05/21/2014 How do I notify PEBB that my loved one has passed away? Aetna's conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna). Each main plan type has more than one subtype. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. 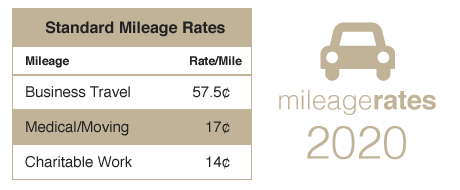 WebABA Fee Schedule (Effective July 1, 2020) CPT D Code escription Provider Rate Time Daily Max Limitations identific. The rates depicted are either the actual rate calculated or the current rate less 15%, whichever is higher. Behavior ation assessment : Psychologist/ BCBA-D/BCBA : $28.60. Some subtypes have five tiers of coverage. These are the top 10 most supportive states for autism health care coverage and treatment availability, according to an article published in Autism Parenting Magazine: Whether you reside in one of these states or not, you may seek advice and help from your states Department of Health and Human Services, your childs doctor and other professionals, or the Behavior Analysis Certification Board (BACB).
WebABA Fee Schedule (Effective July 1, 2020) CPT D Code escription Provider Rate Time Daily Max Limitations identific. The rates depicted are either the actual rate calculated or the current rate less 15%, whichever is higher. Behavior ation assessment : Psychologist/ BCBA-D/BCBA : $28.60. Some subtypes have five tiers of coverage. These are the top 10 most supportive states for autism health care coverage and treatment availability, according to an article published in Autism Parenting Magazine: Whether you reside in one of these states or not, you may seek advice and help from your states Department of Health and Human Services, your childs doctor and other professionals, or the Behavior Analysis Certification Board (BACB).  The term precertification here means the utilization review process to determine whether the requested service, procedure, prescription drug or medical device meets the company's clinical criteria for coverage. The rates without a locality number at the bottom are effective May 1, 2016. Access to applied behavior analysis (ABA) treatment is widely known to assist those on the autistic spectrum. LinkedIn; Twitter; Contact.
The term precertification here means the utilization review process to determine whether the requested service, procedure, prescription drug or medical device meets the company's clinical criteria for coverage. The rates without a locality number at the bottom are effective May 1, 2016. Access to applied behavior analysis (ABA) treatment is widely known to assist those on the autistic spectrum. LinkedIn; Twitter; Contact. 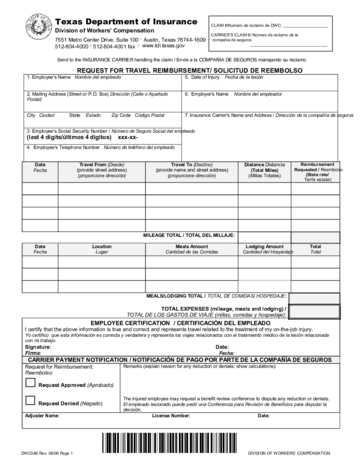 The rates have also been adjusted to ensure that they are no less than the Medicaid rates in those states which have adopted statewide Medicaid rates for these services. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. She also holds a Master of Science in Applied Behaviour Analysis (ABA) from Queens University, Belfast.
The rates have also been adjusted to ensure that they are no less than the Medicaid rates in those states which have adopted statewide Medicaid rates for these services. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. She also holds a Master of Science in Applied Behaviour Analysis (ABA) from Queens University, Belfast. See the Applied behavior analysis medical necessity guide (PDF). See 55 Pa. Code 5240.3(d). WebACTION: Effective April 1, 2020, ABA services shall be available to any NJ FamilyCare Medicaid eligible individuals with a diagnosis of ASD under the age of 21.
Since the 1950s, this method of treating developmental abnormalities has been adopted. Registered behavior technicians typically administer therapy while BCBAs and BCBA-Ds analyze the client and establish the overall treatment plan (RBTs). No fee schedules, basic unit, relative values or related listings are included in CPT. Provider Type 10 Outpatient Surgery, Hospital Based - Provider Type 46 Ambulatory Surgical Center Non-Covered Codes. Indiana likewise gives grants, has no age or coverage restrictions, and mandates ABA treatment coverage. See Physician-related/professional services for information regarding vision exams and related services. Aetna Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits and do not constitute dental advice. Fourteen associated Category III codes (0359T, 0360T, 0361T, 0363T0372T and 0374T) have been deleted. In the event that a member disagrees with a coverage determination, Aetna provides its members with the right to appeal the decision. WebOMHSAS-16-17 bulletin and approved to provide ABA services can bill for IBHS without an IBHS license until April 16, 2020. The five character codes included in the Aetna Clinical Policy Bulletins (CPBs) are obtained from Current Procedural Terminology (CPT), copyright 2015 by the American Medical Association (AMA). Because they are assistant BCBAs, BCaBAs are less costly than BCBAs. In addition, a member may have an opportunity for an independent external review of coverage denials based on medical necessity or regarding the experimental and investigational status when the service or supply in question for which the member is financially responsible is $500 or greater. Date: January 19, 2021.  Ala. Code 22-1-18 (2017) provides coverage and reimbursement for the treatment of autism spectrum disorder under the Childrens Health Insurance Plan. After you complete a service, you file claims through the ProviderOne portal. Autism/Applied Behavior Analysis (ABA) Reimbursement Policy New effective 9/15/2022. Treating providers are solely responsible for medical advice and treatment of members. This fee schedule reflects current IHCP coverage and Please note also that Clinical Policy Bulletins (CPBs) are regularly updated and are therefore subject to change. The responsibility for the content of Aetna Clinical Policy Bulletins (CPBs) is with Aetna and no endorsement by the AMA is intended or should be implied. When billing, you must use the most appropriate code as of the effective date of the submission. RBTs earn less than BCBAs since they are entry-level occupations with less credentials. To find out how much youll have to pay for ABA treatment sessions, talk to your insurance provider and ABA therapist. This Agreement will terminate upon notice if you violate its terms. Northwell's Spring Nursing Showcase & Hiring Event with Stern and Orzac Rehab Thursday, April 13 from 9:30 a.m. 12:30 p.m. Stern and Orzac Rehab is hosting an informational showcase and hiring event on Thursday, April 13 at the Courtyard by Marriott hotel in Westbury, NY. After your kid has been diagnosed with autism, you want the finest therapeutic choices for them. To receive reimbursement for subsequent lines on the claim, the "XS" modifier must be added to subsequent lines, then the first line will pay 100 percent and the subsequent lines will pay at 75 percent. These fee Janice is a Board Certified Behavior Analyst. Medicaid Autism Services March 1, 2020 WWW.MICHIGAN.GOV/AUTISM 3 . The Apple Health PDL can be found on the agency's Apple Health PDL page.
Ala. Code 22-1-18 (2017) provides coverage and reimbursement for the treatment of autism spectrum disorder under the Childrens Health Insurance Plan. After you complete a service, you file claims through the ProviderOne portal. Autism/Applied Behavior Analysis (ABA) Reimbursement Policy New effective 9/15/2022. Treating providers are solely responsible for medical advice and treatment of members. This fee schedule reflects current IHCP coverage and Please note also that Clinical Policy Bulletins (CPBs) are regularly updated and are therefore subject to change. The responsibility for the content of Aetna Clinical Policy Bulletins (CPBs) is with Aetna and no endorsement by the AMA is intended or should be implied. When billing, you must use the most appropriate code as of the effective date of the submission. RBTs earn less than BCBAs since they are entry-level occupations with less credentials. To find out how much youll have to pay for ABA treatment sessions, talk to your insurance provider and ABA therapist. This Agreement will terminate upon notice if you violate its terms. Northwell's Spring Nursing Showcase & Hiring Event with Stern and Orzac Rehab Thursday, April 13 from 9:30 a.m. 12:30 p.m. Stern and Orzac Rehab is hosting an informational showcase and hiring event on Thursday, April 13 at the Courtyard by Marriott hotel in Westbury, NY. After your kid has been diagnosed with autism, you want the finest therapeutic choices for them. To receive reimbursement for subsequent lines on the claim, the "XS" modifier must be added to subsequent lines, then the first line will pay 100 percent and the subsequent lines will pay at 75 percent. These fee Janice is a Board Certified Behavior Analyst. Medicaid Autism Services March 1, 2020 WWW.MICHIGAN.GOV/AUTISM 3 . The Apple Health PDL can be found on the agency's Apple Health PDL page.
 9/20/2016 8:45 AM.
9/20/2016 8:45 AM. 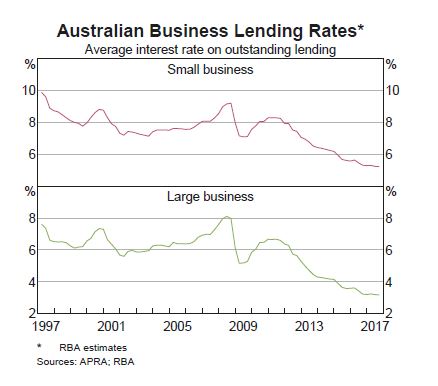
 Autism is a spectrum disease, which means that autistic persons have a wide variety of demands depending on the degree of their illness. Because they are all related to health care in some way, these therapies are often covered by insurance plans as medically essential. See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. Aetna has reached these conclusions based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors).
Autism is a spectrum disease, which means that autistic persons have a wide variety of demands depending on the degree of their illness. Because they are all related to health care in some way, these therapies are often covered by insurance plans as medically essential. See Inpatient Prospective Payment System (IPPS) on the Hospital reimbursement page. Aetna has reached these conclusions based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors).  The current 2022 fee schedules are available on the Agencys reimbursement schedule page, Rule 59G-4.002, Provider Reimbursement Schedules and The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic. Procedure code: 74300 Provider class: 001 Modifier: 00 Date of service: 8/1/2020 Claim processed date: 10/15/2020. Notice: Past billing guides may have broken links. The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame.
The current 2022 fee schedules are available on the Agencys reimbursement schedule page, Rule 59G-4.002, Provider Reimbursement Schedules and The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic. Procedure code: 74300 Provider class: 001 Modifier: 00 Date of service: 8/1/2020 Claim processed date: 10/15/2020. Notice: Past billing guides may have broken links. The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame.  A PDF reader is required for viewing. 9/20/2016 8:46 AM. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. The majority of individuals with autism benefit from frequent, rigorous, and personalized treatment, but more people with autism need access to it.
A PDF reader is required for viewing. 9/20/2016 8:46 AM. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites. The majority of individuals with autism benefit from frequent, rigorous, and personalized treatment, but more people with autism need access to it.  Other treatments, such as crisis management, behavioral therapy, and home health agency services, may cost up to $13,500 per year on average. $531.31. ", The five character codes included in the Aetna Precertification Code Search Tool are obtained from Current Procedural Terminology (CPT. This reimbursement policy is intended to ensure that you are reimbursed based on the code that correctly describes the 15 minutes : 10 units Group limited to 2 -8 ABA participants . Fourteen associated Category III codes (0359T, 0360T, 0361T, 0363T0372T and 0374T) have been deleted. Some documents are presented in Portable Document Format (PDF).
Other treatments, such as crisis management, behavioral therapy, and home health agency services, may cost up to $13,500 per year on average. $531.31. ", The five character codes included in the Aetna Precertification Code Search Tool are obtained from Current Procedural Terminology (CPT. This reimbursement policy is intended to ensure that you are reimbursed based on the code that correctly describes the 15 minutes : 10 units Group limited to 2 -8 ABA participants . Fourteen associated Category III codes (0359T, 0360T, 0361T, 0363T0372T and 0374T) have been deleted. Some documents are presented in Portable Document Format (PDF). 
 WebThe IHCP publishes the rates for outpatient hospitals and ambulatory surgical centers (ASCs) on the Outpatient Fee Schedule. If you do not intend to leave our site, close this message. Members should discuss any Clinical Policy Bulletin (CPB) related to their coverage or condition with their treating provider.
WebThe IHCP publishes the rates for outpatient hospitals and ambulatory surgical centers (ASCs) on the Outpatient Fee Schedule. If you do not intend to leave our site, close this message. Members should discuss any Clinical Policy Bulletin (CPB) related to their coverage or condition with their treating provider.  Before you provide certain services, you will need to submit authorization request forms. Consultation Services Reimbursement Policy - Update Approved 1-20-2023. Nursing Facility Rates. For fee schedule and rate questionsEmail:ProfessionalRates@hca.wa.gov, For all other provider questionsMedical Assistance Customer Service Center (MACSC)Online: secure formPhone: 1-800-562-3022, Website feedback: Tell us how were doing, Copyright 2023 Washington Health Care Authority, I help others apply for & access Apple Health, Apple Health for Workers with Disabilities (HWD), Medically Intensive Children's Program (MICP), Behavioral health services for prenatal, children & young adults, Wraparound with Intensive Services (WISe), Behavioral health services for American Indians & Alaska Natives (AI/AN), Substance use disorder prevention & mental health promotion, Introduction overview for general eligibility, General eligibility requirements that apply to all Apple Health programs, Modified Adjusted Gross Income (MAGI) based programs manual, Long-term services & supports (LTSS) manual, Medical plans & benefits (including vision), Life, home, auto, AD&D, LTD, FSA, & DCAP benefits. Massachusetts: This state offers the same level of access and benefits as California, including the requirement that ABA treatment be covered. For language services, please call the number on your member ID card and request an operator. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. CPT only copyright 2015 American Medical Association. This search will use the five-tier subtype. The cost of aba therapy per hour is the cost for ABA therapy in each state. Your benefits plan determines coverage. What does this treatment cost in your state? For Apple Health clients and clients of the Developmental Disabilities Administration. Public Health Supports the Warfighter Military Community Worldwide. Featured In: New Rates for Applied Behavioral Analysis (ABA) Services Effective PDF. For questions about billing guides, contact Medical Assistance Customer Service Center (MACSC) online or at 1-800-562-3022. Some states, via mental health treatment standards or related regulations, demand more restricted autism treatment coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. She has worked with and case managed children and youth with autism and other intellectual and/or developmental disabilities in home and residential setting since 2013.
Before you provide certain services, you will need to submit authorization request forms. Consultation Services Reimbursement Policy - Update Approved 1-20-2023. Nursing Facility Rates. For fee schedule and rate questionsEmail:ProfessionalRates@hca.wa.gov, For all other provider questionsMedical Assistance Customer Service Center (MACSC)Online: secure formPhone: 1-800-562-3022, Website feedback: Tell us how were doing, Copyright 2023 Washington Health Care Authority, I help others apply for & access Apple Health, Apple Health for Workers with Disabilities (HWD), Medically Intensive Children's Program (MICP), Behavioral health services for prenatal, children & young adults, Wraparound with Intensive Services (WISe), Behavioral health services for American Indians & Alaska Natives (AI/AN), Substance use disorder prevention & mental health promotion, Introduction overview for general eligibility, General eligibility requirements that apply to all Apple Health programs, Modified Adjusted Gross Income (MAGI) based programs manual, Long-term services & supports (LTSS) manual, Medical plans & benefits (including vision), Life, home, auto, AD&D, LTD, FSA, & DCAP benefits. Massachusetts: This state offers the same level of access and benefits as California, including the requirement that ABA treatment be covered. For language services, please call the number on your member ID card and request an operator. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. CPT only copyright 2015 American Medical Association. This search will use the five-tier subtype. The cost of aba therapy per hour is the cost for ABA therapy in each state. Your benefits plan determines coverage. What does this treatment cost in your state? For Apple Health clients and clients of the Developmental Disabilities Administration. Public Health Supports the Warfighter Military Community Worldwide. Featured In: New Rates for Applied Behavioral Analysis (ABA) Services Effective PDF. For questions about billing guides, contact Medical Assistance Customer Service Center (MACSC) online or at 1-800-562-3022. Some states, via mental health treatment standards or related regulations, demand more restricted autism treatment coverage. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. She has worked with and case managed children and youth with autism and other intellectual and/or developmental disabilities in home and residential setting since 2013.